Carcinoma lung with pleural effusion
04 SEP 2010
Carcinoma lung with pleural effusion
Authors:
Sajid Abdul Majid; PGY 2, PGMEM
Binu Kuriakose ; PGY 1, PGMEM
Fabith Moideen VM; Attending ER Physician
Venugopalan P.P (HOD, EM)
A 80 year old female a known case of CAD, systemic hypertension
and COPD presented to the emergency department with complaints of
progressive dyspnoea since 1 month which worsened over the past
3 days and altered sensorium of 2 days duration.
Symptoms:
Presented with
Dyspnoea - 1 month which worsened over the past 3 days
Altered mental status - 2 days
Allergies: None
Medications:
T.Ecospirin 150mg 0-1-0
T.Clopilet 75mg 1-0-0
T.Nicardia R 10mg 1-0-1
Past medical/surgical history:
CAD - 8 years
Systemic hypertension – 8 years
COPD – 6 years
Last meal: 10 pm, dinner
Event:
•progressive dyspnoea which worsened over the past 3 days
•Altered sensorium - 2 days
Airway: Patent
Breathing:
Respiratory rate: 30/min
Air entry decreased over right side
Circulation:
Pulse: 132/min regular
BP: 130/90 mm of Hg
Normal Capillary refill
Disability: Responsive to pain, pupils reactive bilateral
Exposure: No rashes
Vitals: Temp - 96.50F
Pulse - 132/min regular
BP - 130/90 mm of Hg
Respiratory rate - 30/min
SpO2 - 90% with 4L of O2
Head to toe examination:
Thin built, normal stature
Pallor +
Neck: Trachea shifted to right, accessory muscles of respiration +
No JVD, No lymphadenopathy
Chest : Respiratory movements decreased over right side
Air entry decreased over right upper and lower zones
Dull note on percussion over right side
CVS: S1 S2 normal, No rubs
P/A: soft, non-distended
No hepatosplenomegaly
BS +
External genitalia: Normal
Extremities: No edema, Peripheral pulses +
Neurology: Responsive to pain; cranial nerves, motor,
sensory and reflexes – could not be assessed
No signs of Meningeal Irritation.
Differential diagnosis:
Right lung collapse with pleural effusion
Carcinoma lung
Labs:
CBC – Hb: 11.2g%
WBC count: 10,600/cmm
DC: Polymorphs-55
Lymphocytes-34
Basophils-8
Monocytes-1
Platelets: 3.1 lakhs/cmm
Chest Xray AP view

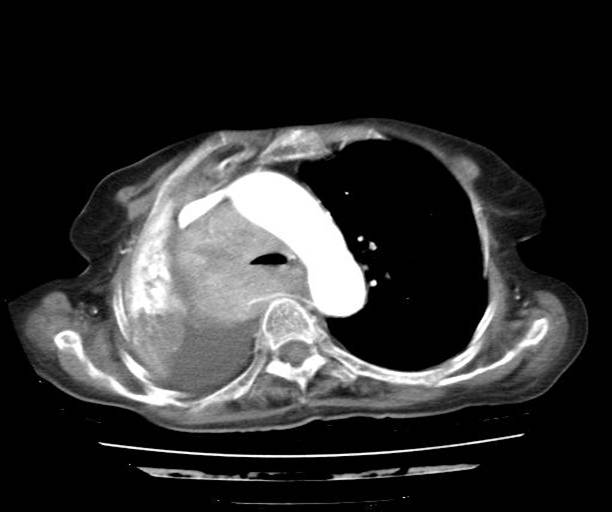
CT thorax
.jpg)
DISCUSSION CARCINOMA LUNG
Bronchogenic carcinoma is the most common visceral malignancy
malignancy related deaths in females.
Etiology & Pathology:-
1. Tobacco smoking: As per many studies and statistical analysis
done in the past, cigarette smoking has been considered as the
most common agent related to Ca lung1
-It has been related to no.of pack yrs and tendency to inhale the smoke.
-More than 40 cigarettes per day for 10 yrs increases chances of Ca
lung upto several folds1
-Similarly cessation of smoking decreases the risk by several folds
-Tobacco has been implicated in many othe cancers like Lip, tongue,
Floor of the mouth, Pharynx, Larynx,Esophagus,Urinary bladder,Prostate,Kidney
-More then 1200 carcinogens have been isolated from tobacco
2. Industrial Hazards: All types of radiation are related to lung cancers
-The survivors of Hiroshima, Nagasaki had increased incidence of lung cancers.
-Uranium miners commonly have lung cancers after 10-20 yrs of work.
-Other potential causes includes: Asbestos, Nickel , Chromates, Coal,
Mustard gas, Arsenic, Beryllium etc.
3. Air Pollution: Very potential cause for Ca lung as has been seen in
Many developing nad developed countries
4. Molecular genetics: Many oncogenes are implicated in development of Ca lung
- C-myc is seen in small carcinoma , K-ras in adenocarcinoma
-P53 . Retinoblastoma are also seen
5. Scarring: In the vicinity of Pulmonary scars, there can be adenocarcinoma
Histological classification:
-Small cell carcinoma
-Adenocarcinoma:Bronchial , Bronchoalveolar , Acinar
-Small cell carcinoma:Oat cell carcinoma , Intermediate cell
-Combined cell carcinoma
Revised International staging for Ca lung
T1:Tumour 3 cm without plueral or main stem bronchus involvement
T2:Tumour 3 cm or involvement of main stem bronchus 2 cm from
carina, viseral , pleural or lobar atelectasis.
T3:Tumour with invasion of mediastinum , heart, great vessels,
trachea,esophagus, vertebral body or malignant pleural effusion.
N0:No nodal involment
N1:I/L Hilar or peribronchial node involvement
N2:I/L Mediastinal or subcarinal lymph nodes
N3:C/L Mediastinal or hilar lymph nodes, or I/L or
C/L Scalene or supraclavicular lymph nodes
M0:No metastasis
M1:Distant metastasis
Stage Staging 5 yr Survival rate
1a T1N0M0 >70
1b T2N0M0 60
2a T1N1M0 50
2b T2N1M0 30
T3N0M0 40
3a AnyTN2M0 10-30
T3N1M0 10-30
3b AnyTN3M0 <10
T4AnyNM0
4 AnyTAnyNM1 <5
COMMON SIGNS & SYMPTOMS OF LUNG CANCER
*Symptoms secondary to central or endobronchial growth of primary tumours
-Cough
-Wheeze & Stridor
-Pnemonitis from obstruction
-Hemoptysis
-Dyspnoea from obstruction
*Symptoms sec. to Peripheral growth of primary tumour
-Pain from pleural or chest wall involvement
-Cough
-Dyspnoea
-Lung abscess syndromes
*Symptoms related to regional spread of tumors in thorax by
contiguity or by mets of regional Lymph node
-Tracheal obstruction
-Esophageal compression dysphagia
-Horners syndrome
-Right Laryngeal nerve paralysis with hoarseness
-Phrenic nerve paralysis wit hemidiaphragm elevation
-Pancoast syndrome
-SVC Obstruction
-Lymphatic obstruction with plueral effusion
PARANEOPLASTIC SYNDROMES
1)Endocrine: Hypercalcemia; Cushings syndrome; SIADH;
Carcinoid syndrome; Gynaecomastia; Hypoglycemia; Hyperthyroidism
2)Neurological: Encephalitis; Subacute cerebellar degeneration;
Progressive multifocal leukoencephalitis;Peripheral neuropathy;
Polymyositis; Eaton Lambort; Optic Neuritis
3)Skeletal:Clubbing; Pul. Hypertrophic osteoarthropathy
4)Haemat:Anaemia; Leukemoid Rxn; Thrombocytosis;Thrombocytopenia:DIC
5)Cutaneous:Hyperkratosis; Dermatomyositis;
Acanthosis nigricans;Erythema gyratum repens
6)Nephrotic syndromes; Hypouricemia; Anorexia; Cachexia
WORK UP FOR EVALUATION3
1. Imaging:
a)CXR:A Perfectly normal CXR does not exclude lung ca;
as conventional CXR may not always identify hilar or mediastinal lesions
- Lung ca can present as mass, peripheral nodule; or pleural effusion
b)CT Scan:Most effective non invasive modality of choice
-Also helps identify local invasion (chest wall , bones, pleura)
c)MRI:Not routinely used, but in suspected spinal cord
compression,brachial plexus or chest wall involvement
d)Fluorodeoxyglucose(FDG); PET scan
2. Pathological diagnosis:
-Flexible fibreoptic bronchoscopy can help determine extent of
endobronchial lesions and to obtain tissue foe diagnosis
-Cytological examination for patients in CT & Bronchoscopy cannot be done
-Mediastinoscopy is very useful to determine status of mediastinal
lymphnodes for patients who are candidates for surgical resection
-VATS can be used to acess peripheral nodes or suspected pleural effusion
TREATMENT MODALITIES
1.CHEMOTHERAPY
2.RADIOTHERAPY
1)Chemotherapy: Drugs used are
-Paclitaxel -Carboplatin -Etoposide
-Cisplatin -Vinorelbine -Gemcitabine
2)Radiotherapy:
-Administration of thoracic RT in conjunction with systemic
chemotherapy has shown improvement
EMERGENT COMPLICATION
1)Malignant pleural effusion with tamponade
-Sudden accumulation of fluid or hemorrhage may cause
dyspnoea, chest pain, hypotension
-C/F of cardiac tamponade:
-Hypotension & narrow pulse pressure
-JVD
-Low QRS on ECG
-Decreased heart sounds
-Pulsus paradoxus
-Cardiomegaly without features of CHF
-Emergency Pericadiocentesis is treatment of choice.
It is safe, effective and well tolerated.
REFERENCES
1.Robbins pathologic basis of Disease: Kumar, Collins
2.Cancer principles & Practice of oncology; Devatti
3.Washingtons manual of oncology
4.Emergency medicine; Tintinalli 6th edition