Purulent Pericardial effusion in Retro Virus infection
08 FEB 2013
PURULENT PERICARDIAL EFFUSION
Alex A -PGY 1
Fabith MoideenDeputy- Chief , Ramanidharan- Faculty, Harshad- PGY2
Venugopalan .P.P Chief
38 yr old male, was brought in to the Emergency Department with complaints of
retrosternal chest pain since 15 days.
General Impression: Conscious, oriented.
Primary survey:
Airway – patent, no obstruction
Breathing – air entry B/L equal, no added sounds.
Circulation-CRT-< 2 sec, peripheral pulses equal and felt.
Disability –alert, conscious, moving all limbs.
Exposure –.Bilateral pitting pedal edema, redness over foot bilaterally
Vitals:
BP-110/70 PR-124 SPO2-98 on room air, TEMP-afebrile RR- 18 GRBS-147
PAIN SCORE-3/10
Signs and symptoms-H/o - Retrosternal chest pain which Increase on coughing , deep
inspiration and leaning forward since 15 days . Constant pain .
No dyspnea .No radiation to neck , arms , back .
H/o fever, cough, loose stools for 4 days. , Fever mild to moderate grade not associated
with chills and rigors. h/o odynophagia +
Also gives h/o significant Wt loss . Decreased appetite . Fatigue +
Pedal edema + 1 day, redness over foot bilaterally
oral antibiotics .
Past Medical /Surgical History-
chronic smoker and chronic alcoholic
No other significant history
Last Meal: lunch, 3 pm
Events:in Nigeria, as an x ray welder, irregular meal timings, long fasting hours
between meals, skips dinner and has two meals per day. He received treatment from a
local general practitioner after which he found no relief, hence he came here to MIMS for
further management.
Head to Toeexamination
HEENT- normal
Trachea – central
JVD- normal
Chest – b/l air entry equal , no added sounds.
PA- soft, lax , BS +
CNS- conscious, alert, HMF – normal. Moving all limbs.
CVS- S1S2 ++, no murmurs.
INTIAL MANAGEMENT:
IV access
O2 – 4 lit with face mask
MONITOR: normal sinus rhythm.
Vitals rechecked,
Blood samples collected
Drugs administered :
• Inj pantocid 40 mg iv
• Tab ecospirin 300 mg p/o
• Tab clavix 300 mg p/o
Point of Care Ultrasound :
Pericardial effusion+.
Moderate LV dysfunction
No pneumothorax.
IVC: Normal
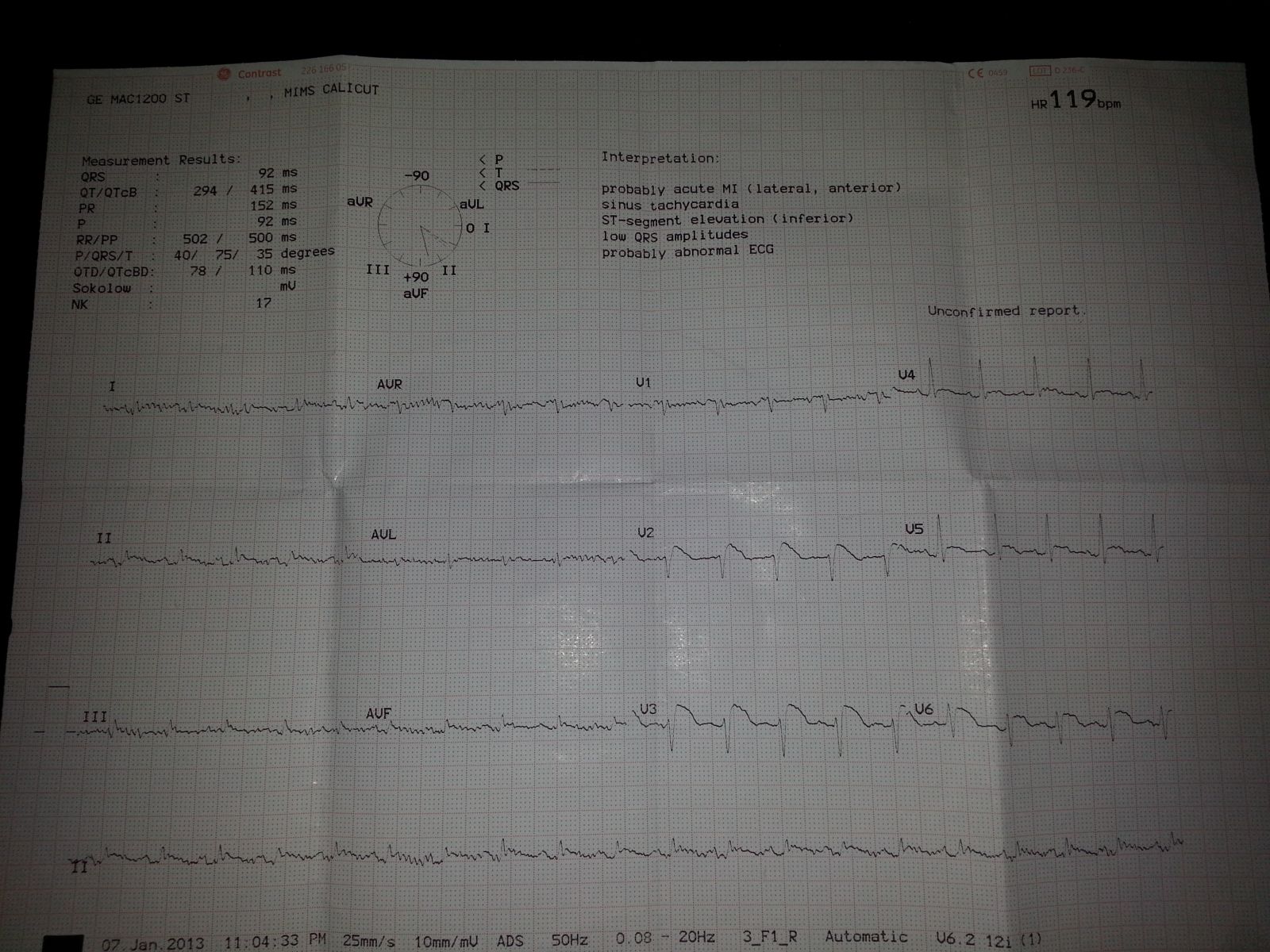
ECG-Sinus tachycardia , ST elevation in all leads except avR & V1
( Convex - upwards ST elevation ) ,PR – Normal.
D/D:
Pericarditis
Acute coronary syndrome
Lower Respiratory Tract Infection
Cardiac tamponade
Aortic dissection
Acute gastritis/Duodenal ulcer.
Oesophageal rupture
Oesophagitis
Pneumothorax
Pulmonary embolism
Costochondritis
Initial diagnosis:
Pyrexia of Unknown Origin
Possible Myocarditis / Pericarditis
INVESTIGATIONS
GRBS: 138 mg/dL
HIV 1 & 2[Card & ELISA]: POSITIVE / HBsAg [Card]: Negative / HCV [Card]: Negative /
VDRL: Negative
Peripheral smear: 1. Mild normocytic normochromic anemia. 2. Neutrophilic
leukocytosis
Pericardial fluid cytology: No malignant cells seen
Pericardial fluid culture: Staphylococcus aureus
Pericardial fluid Gram-Stain: Few Gram positive coccoid forms noted
Chest X-ray
Cardiac enlargement +
ECG -Sinus tachycardia, ST elevation in all leads except aVR and V1
ECHO
[on admission]: No RWMA. Valves normal
Normal biventricular function. LVEF = 55-60 %
No clots. Pericardial effusion + (2 cm in any direction)
No intra-cardiac clots. IVC dilated. Respiratory movements present
[pre-discharge]: Mild-to-moderate pericardial effusion with strands
No RA / RV collapse. No RWMA. Normal LV & RV function. LVEF - 55-60 %
Normal valves. Trivial mitral regurgitation


CT Thorax:
Moderate pericardial effusion. Small left pleural effusion
COURSE IN THE HOSPITAL
This gentleman, admitted with atypical chest pain and fever, was found to have large
pericardial effusion on echocardiogram and was hence admitted for further evaluation
and management. Blood investigations showed leukocytosis, neutrophilia and high
ESR. He was also found to be positive for retroviral antibodies. He was taken up for
pericardiocentesis and drained purulent pericardial fluid. Pericardial fluid culture grew
Staphylococcus aureus and antibiotics were started according to sensitivity. He was
afebrile since 12-01-2013. However, a repeat echo done showed re-accumulation of
pericardial fluid and underwent pericardiocentesis two further times during subsequent
hospital stay. A spiral CT scan thorax done did not show any evidence of mediastinal
lymphadenopathy / mass lesion. He was started on anti-retroviral therapy in consultation
with our Microbiologist. His Cryptococcal antigen test, PCR for TB, toxoplasma IgG
results are awaited. VDRL test was non-reactive. HIV viral load testing and CD4 + count
testing were also done – reports are awaited. He is advised to continue treatment from
local hospital. Antibiotics should be continued for 1 more week. I.V Gentamicin was
stopped after completing 15 days of therapy. At the time of discharge, he continued to
have moderate-to-large pericardial effusion with evidence of systemic venous congestion.
He is likely to require surgical intervention for pericardial effusion.
FINAL DIAGNOSIS:
LARGE PURULENT PERICARDIAL EFFUSION
SECONDARY DIAGNOSIS
RETROVIRAL POSITIVE STATE
Discussion
Purulent pericardial effusion :
Purulent(or suppurative) pericarditis is defined as an infection of
the pericardial space that produces pus Bacterial infections of the
pericardium are relatively uncommon but are much more likely to produce
purulent effusions and to proceed to cardiac tamponade and pericardial
constriction.
Purulent pericarditis occurs almost exclusively as a secondary infection in
patients with serious underlying disease, including patients with AIDS and
those undergoing hemodialysis, thoracic surgery, and chemotherapy.
Bacterial pericarditis has a high mortality rate despite appropriate therapy
(30%–50%), with the majority of deaths due to cardiac tamponade.
The reported incidence of pericardial involvement among patients with
pulmonary tuberculosis ranges from 1% to 8%; however, evidence of
active pulmonary disease is uncommon, with only 11% to 50% of patients
with tuberculous pericarditis having positive sputum cultures.
• Pericardial involvement can occur with a primary infection, reactivation of
latent infection, and during appropriate antitubercular therapy.
• The most common pathway is retrograde extension via lymphatics from
peribronchial and mediastinal nodes; other recognized pathways include
hematogenous spread from a distant foci (genitourinary or skeletal) and
direct extension from a contiguous source (lymph nodes, lung, pleura,
spine).
• Four pathologic stages of tuberculous pericarditis
have been identified:
(1) fibrin deposition with many polymorphonuclear neutrophils and
abundant
organisms as well as loose granuloma formation;
(2) accumulation of serosanguinous effusion with predominating
lymphocytes
and monocytes;
(3) absorption of the effusion, with a reduction in the number of
Mycobacterium
tuberculosis organisms and thickening of the pericardium due to the
formation
of dense caseating granulomas;
(4) replacement of granulomas by fibrous tissue, which begins to
Calcification may occur at any pathologic stage.
HIV Infection
• An estimated 6% to 7% of patients with HIV infection experience
significant HIV-related cardiac morbidity, and pericardial effusion and
myocarditis are the most common.
• Approximately 25% of HIV patients with advanced disease have an
effusion by echocardiography, and 20% of these effusions were large.
• The majority of patients were asymptomatic, and at follow-up 42% of the
effusions had resolved spontaneously.
• In a series of patients requiring intervention for tamponade, the most
common underlying disorders were malignancy and HIV.
• Pericardial disease can result from opportunistic infections, medical
treatment of HIV infection, and the HIV infection itself. In these
immunocompromised patients, one must consider not only viral and
bacterial pathogens, but also fungal, mycobacterial, and parasitic
(Toxoplasma gondii) infections.
• Noninfectious causes include lymphoma and Kaposi sarcoma.
• The risk factors associated with moderate-severe pericardial effusion
in patients with HIV infection were tuberculosis heart failure other
pulmonary infection , and Kaposi sarcoma.
• Thus, it is prudent to initiate empirical treatment for tuberculosis in a
patient with HIV who is symptomatic with a persistent pericardial effusion
until that diagnosis can be confirmed or excluded.
Lessons Learnt :
Purulent pericarditis is nearly always a complication of another infection,
and a high level of suspicion is needed to make the diagnosis.
In treating suspected bacterial pericarditis, broadspectrum antibiotics with
anaerobic coverage should be used until the microbe is identified.
Tachycardia is a sensitive but nonspecific sign of pericardial disease that
may signal early tamponade physiology
Hypotensive patients should be checked for pulsus paradoxus (especially
if they have jugular venous distention); if present, an echocardiogram
should be obtained.
A multidisciplinary approach including infectious disease,
cardiology,pulmonology and cardiothoracic surgery is optimal for making
the diagnosis of and providing the treatment for complex pericardial
infections.
References:
1) Rosen’s Textbook of Emergency Medicine (7th Edition)
2) Tintinally’s textbook of Emergency Medicine (7th Edition)
3) Harrison’s Principles of Internal Medicine – 4th Edition
4) Online references (Uptodate- Purulent pericardial effusion, ACEP Journal )