Migrating Bullet
12 MAY 2014
The Curious Case of a Migrating Bullet
Dr Hafeez T, MEM PGY2, MIMS Calicut
Dr Shibu Varghese, Deputy Chief, Emergency Medicine
Dr Venugopalan P.P, Head of Department
Editor: Dr Lajeesh Jabbar, MIEM
Emergency room presentation
A 72 year old male presented to our emergency department with alleged h/o accidental gunshot injury. He reported having been shot in his neck. On arrival to ED he had stable vital signs. His primary survey was unremarkable, on exposure he had a small entry wound over the right side of neck in zone 2. E-FAST and Chest X rays were normal. He only complained of a small wound and mild pain over right side of neck which he sustained after an accidental gunshot injury with an airgun 2 hours back. There was no bleeding from the wound. He had no allergies. He was a known case of Type 2 DM, Hypertension and CAD on OHA, antihypertensive and antiplatelet.
Head to Toe was unremarkable except for a 1 x 1cm entry wound over the right sternocleidomastoid in zone 2 with a surrounding hematoma.
.jpg)
Investigations
CBC: HB – 14.5, TC – 13000, Neutrophils – 70%
Creatinine: 1.5
RBS: 180mg/dl
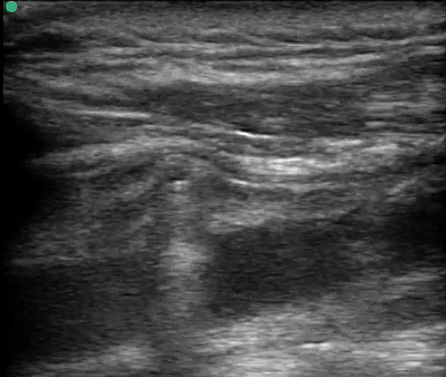
POC Ultrasound neck done in ED showed the bullet lying anterior to the IJV.
X Ray Neck showed the bullet anterior to the lower border of C6 Vertebra.
CT Neck showed metallic foreign body piercing the right sternocleidomastoid muscle at the level of lower border of C6 vertebral body, likely abutting the carotid sheath at the level of lower border of cricoid cartilage on right side of neck. Soft tissue density anterior to IJV and CCA -likely haematoma
.jpg)
.jpg)
.jpg)
Disposition
Consultation with ENT Surgeon was obtained and the patient was posted for neck exploration and foreign body removal under GA the next morning.
Course in Hospital
The patient was taken to OT the next day. Right neck was explored with vertical incision, there was a small haematoma around carotid sheath, but the FB was not located in the neck, C arm done showed the FB in thorax at the level of 4th rib. The neck wound was sutured and the patient was shifted to SICU.
A CT Thorax was done which showed the metallic pellet migrated through internal jugular vein into inferior
venacava atrial junction.

On consultation with the Cardiothoracic Surgeon it was the advised that the patient will require cardiopulmonary bypass and cardioplegic arrest to retrieve the foreign body. But considering the high risk nature of the surgery, the patient relatives were not keen for it. Hence it was decided to manage the patient conservatively.
The next day a fluoroscopic examination was done and pellet was located in the left common iliac vein and subsequently in right external iliac vein. The pellet was snared in the vein and delivered through a small venotomy with the help of interventional cardiologists. The patient remained stable throughout the post-operative period and was discharged home on the 4th day of admission.
Discussion
This case reports an unusual and potentially serious complication of a bullet embolising through the venous system and to the heart. Migration of a bullet from its initial location to a distant site has been rarely reported, and migration to the heart is even rarer. After a gunshot, except for a penetrating injury, the bullet usually remains at the original location and only occasionally migrates toward other body parts. A bullet may migrate via several routes. It may migrate locally along the intermuscular space or lumen, or it may migrate along the vein or artery to a distant site.
The scenario for bullet embolism is set up when a low-velocity projectile consumes enough kinetic energy on the initial tissue penetration such that it only penetrates a single wall of a vessel, coming to rest within the lumen. This occurs most commonly with small-caliber, relatively low-powered projectiles such as BBs, 0.22 caliber bullets, airgun pellets or shotguns ammunition, which scatters multiple small metallic pellets. Forces, which then influence the migration of an intravascular foreign body include: Hydrostatic pressure from blood flow, gravity, patient body position, and vascular anatomy. Embolization is also more commonly encountered in the arterial system than in the venous system. Reports of venous involvement account for just 20-25% of cases. Most venous projectiles embolize from peripheral sites to the heart or vena cava (antegrade migration), but they can also migrate in a retrograde direction.
The treatment for bullet retention and migration is inconclusive. Bullets remaining in the human body may cause various complications, such as pain, local paresthesia, claudication, gangrene, bullet-induced toxicity, thrombophlebitis, pericardial/pleural effusion, pulmonary abscess/infarction, endocarditis, arrhythmia, false aneurysm, septicemia, cerebral infarction, and mental abnormalities. When bullet embolization is suspected, management will depend on hemodynamic status, and will usually begin with a CT scan and angiography, the patient’s clinical condition permitting. Intravascular ultrasonography can also be considered if an intraluminal location is suspected. There is little consensus on treatment and indications for removal of bullet emboli, especially from venous sites. However, most authors recommend conservative treatment in asymptomatic patients and recommend surgical removal of the bullet when there are symptoms or if there is a possibility of complications from leaving it in place.
In the case reported herein, the bullet entry was through neck and subsequently lodged within the inferior vena cava (IVC) while the patient remained completely asymptomatic. This bullet changed positions and moved freely within the IVC and the common iliac veins and was finally removed from right external iliac vein by venotomy with the help of interventional cardiologists.
Conclusion
-
Bullet embolism is a rare event and should be suspected when the bullet is not found in the expected location on imaging.
-
Awareness that bullets can move freely within the vascular system may prevent serious complications, including embolization and ischemia.
-
Repeated imaging may be required to find the exact location of bullet and to plan further management.
-
Most of the time, the patients are asymptomatic and only require conservative treatment, but can be appropriately treated by minimally invasive techniques with low morbidity and mortality rates whenever necessary.
-
This was a case of a patient with asymptomatic venous bullet embolism in whom diagnostic methods were able to screen and locate the bullet in the right external iliac vein, allowing safe clinical treatment.
References
-
Kalimi R, Angus LD, Gerold T, DiGiacomo JC, Weltman D. Bullet embolization from the left internal iliac vein to the right ventricle. J Trauma 2002; 52: 772–74.
-
Ronsivalle J, Statler J, Venbrux AC, Arepally A. Intravascular bullet migration: a report of two cases. Mil Med 2005; 170: 1044–47.
-
Bett N, Walters L. Delayed presentation of right ventricular bullet embolus. Heart 2004; 90: 1298.
-
Bertholdo U, Enrichens F, Comba A, Ghiselli G, Vaccarisi S, Ferraris M. Retrograde venous bullet embolism; a rare occurrence case report and literature review. J Trauma 2004; 57: 187–92.
-
Symbas PN, Harlaftis N. Bullet emboli in the pulmonary and systemic arteries. Ann Surg 1977;185:318-20
-
Schroeder ME, Pryor II HI, Chun AK, Rahbar R, Arora S, Vaziri K. Retrograde migration and endovascular ret -5. PMid:21215588.
-
Shannon FL, McCroskey BL, Moore EE, Moore FA. Venous bullet embolism: rationale for mandatory extraction. J Trauma 1987; 27: 1118-1122.
-
Barrett NR. Foreign bodies in the cardiovascular system. Br J Surg 1950; 37: 416-445.
-
Wales L, Jenkins DP, Smith PL. Delayed presentation of right ventricular bullet embolus. Ann Thorac Surg 2001; 72: 619-620.
-
LU Xiao-hui et al Chinese Medical Journal 2011;124(10):1590-1592