Mesenteric ischaemia
13 MAY 2011
Tricky presenation ...Challenge for emergency physicain
Dr. Nihar Lokur
Dr. Shahul Hameed
Dr. Venugopalan P P
74-year-old male was brought to MIMS Emergency department with H/O Back ache since 4 days and pain abdomen since 1 day. He also developed shortness of breath since 4 hrs.
A-Airway patent and Maintainable
B-Breathing fast and b/l ronchi heard
C-Circulation Pulse was irregularly irregular at the rate of 112/min, reduced Right femoral pulse and distal pulses compared to left.
IV access done,O2 and monitor attached
Vitals-SPO2-86% RA and 95% with 6L O2 by face mask,BP-210/130mm of Hg,RR-33/min,HR-112/min irregular,GRBS-189mg/dl,Temp-98.6deg f.
Apart from the symptoms said above, he did not give any history of fever, vomiting, loose stools, multiple joint aches. He said that he had not passed stools since yesterday.
No known allergies
His past medical history is very significant. He is a known case of Hypertension(10 yrs), Atrial Fib with FVR, COPD, CRF(3yrs) and recent h/o CVA (4 months ago)
He was only on anti hypertensives. Other medications he had discontinued since 6 months for reasons not known.
On Examination
Conscious but dyspneic
No pallor, icterus, cyanosis, lymphadenopathy,
No distended neck veins, trachea central
Normal Heart sounds. No added sounds or murmurs.
Respiratory System- expiratory ronchi’s heard on either side.
Abdomen is uniformly distended and generalised guarding observed, bowel sounds sluggish, no signs of free fluid. Inguinal region and external genitals appear normal.
Back- no midline tenderness
Extremities – reduced Right femoral pulse and distal pulses compared to left. Minimal b/l pedal edema+
ECG-Rate 110, tachycardia with Atrial Fibrillation with T inversion in I, aVl and V4-V5
Emergency basic labs were sent with CBC, ESR, Renal Function Test, electrolytes and Urine routine.
Abdominal USG showed abdominal aortic aneurysm of width 4.2cms with intraluminal thrombus with multiple renal calculi.
RT was put to decompress the stomach and foul smelling brown coloured aspirate was seen.
Pain was managed with morphine and fluids were initiated.
Lab results: total counts were elevated, deranged renal parameters and Urine pus cells and Rbc’s present. ABG showed severe metabolic acidosis.
Patient was shifted to ICU and Vascular surgeon, Gastro surgeon consultation was taken .
Working diagnosis-
-AAA
-Renal calculi
-Mesenteric ischaemia
-Sepsis with ARDS
ICU course
Patient was planned to obtain a CECT Abdomen but owing to the deranged renal parameters, it was deferred. Plain CT abdomen was hence taken which showed AAA and multiple renal calculi.Patient was planned for emergency laparotomy. It showed extensive small bowel gangrene extending from the DJ flexure upto the mid transverse colon. Mesenteric pulsations were absent and purulent foul smelling fluid in peritoneal cavity. Findings were discussed with the relatives and poor prognosis explained and the procedure abandoned. The post op period was critical as he was on a ventilator and his vitals started to deteriorate within hours of surgery. Eventually the patient expired.
CT Image
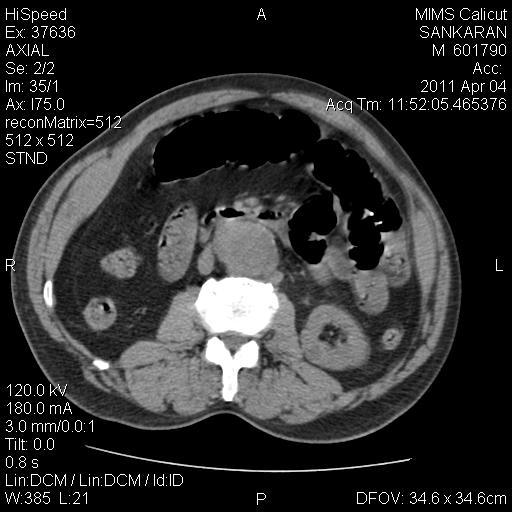
Abdominal aortic aneurysm with maximum width of 4.8cm starting approximately at the level of left renal artery upto bifurcation
Take home lesson
1) Patient having Atrial fibrillation and complaints of pain abdomen, think of MESENTERIC ISCHAEMIA first..
DISCUSSION:
Mesenteric ischaemia is a rare, potentially life threatening disease. First described by Antonio Hodgson in the 15th century but it was studied extensively only from 19th century! It is nothing but disruption of blood flow by an embolus or progressive thrombosis in a major artery supplying the intestine.
Risk factors for acute arterial ischemia include atrial fibrillation, recent myocardial infarction, valvular heart disease, and recent cardiac or vascular catheterization, protein C or S deficiency, antithrombin III deficiency, polycythemia vera, and carcinoma.
Protective responses to prevent intestinal ischemia include abundant collateralization, auto-regulation of blood flow, and the ability to increase oxygen extraction from the blood.
Acute mesenteric ischemia resulting from arterial embolus or thrombosis presents with severe acute, nonremitting abdominal pain strikingly out of proportion to the physical findings. Associated symptoms may include nausea and vomiting, transient diarrhea, and bloody stools. With the exception of minimal abdominal distention and hypoactive bowel sounds, early abdominal examination is unimpressive.
Diagnostic modalities that may be useful in diagnosis but should not delay surgical therapy include ECG, abdominal radiographs, CT, and mesenteric angiography. More recently, mesentery duplex scanning has been demonstrated to be beneficial. The ECG may demonstrate an arrhythmia. A plain abdominal film may show evidence of free intraperitoneal air. Early features of intestinal ischemia on abdominal radiographs include bowel-wall edema, known as "thumb printing." If the ischemia progresses, air can be seen within the bowel wall (pneumatosis intestinalis). CECT with three-dimensional reconstruction is a highly sensitive test for intestinal ischemia. But the "gold standard" for the diagnosis and management of acute arterial occlusive disease is “laparotomy”.
After the initial stabilization, there is a need for urgent laparotomy, emergent admission to a monitored bed or intensive care unit for further evaluation. Aggressive fluid resuscitation is necessary. Broad-spectrum antibiotics should be given to provide sufficient coverage for enteric pathogens, including gram-negative and anaerobic organisms. The goal of operative exploration is to resect compromised bowel and restore blood supply.
Frequent monitoring of the patient's vital signs, urine output, blood gases, and lactate levels is paramount, as is frequent abdominal examination.
If doubt persists, second look laparotomy performed 24–48 h following surgery will allow demarcation of nonviable bowel.
Reference:
Harrison's Principles of Internal Medicine 17th edition, Chp. 292 'Mesenteric vascular insufficiency'
Sabiston Textbook of Surgery 17th edition, Chp. 42 'Acute abdomen'
Medscape online (emedicine.medscape.com)
Rosen's emergency medicine 7th edition, Chp 79 'Lower GI Bleeding'